An introduction to Glutaric Aciduria Type 1 (GA1)
This is an introduction to Glutaric Aciduria Type 1 (GA1), following a diagnosis of your child with this condition.
This is an introduction to GA1 following a positive newborn screening for your child and the management up until 6 years of age.
Consult your metabolic team for diagnosis and treatment for GA1.
This is not designed to replace any advice given by the metabolic team at the hospital.
If you are unclear about anything written on this page, please ask your dietitian for further information.
This guide was written with Prof Anita MacDonald who is a metabolic dietitian from Birmingham Children’s Hospital, who has over 40 years of experience working with parents/carers and children with GA1.
What is GA1?
Glutaric Aciduria Type 1 or GA1 for short
It is pronounced glue-ta-ric-acid-ur-eea
If left untreated, chemicals in the blood build up to toxic levels.
The buildup of harmful substances in the blood can cause movement problems leading to difficulties with walking, talking and swallowing.
GA1 can be life threatening if left untreated.
In newborn diagnosed with GA1, early treatment can prevent these symptoms from occurring and with the correct management your child can have a good quality of life.
Diagnosis of GA1
This blood test (heel prick test) is carried out by a healthcare professional after birth.
High levels of a chemical called glutaric acid are found in the blood.
Diagnosis is confirmed with further blood and urine tests.
Once diagnosed the child will be referred to a specialist metabolic centre to ensure they receive the care they need.
Why does my child have GA1?
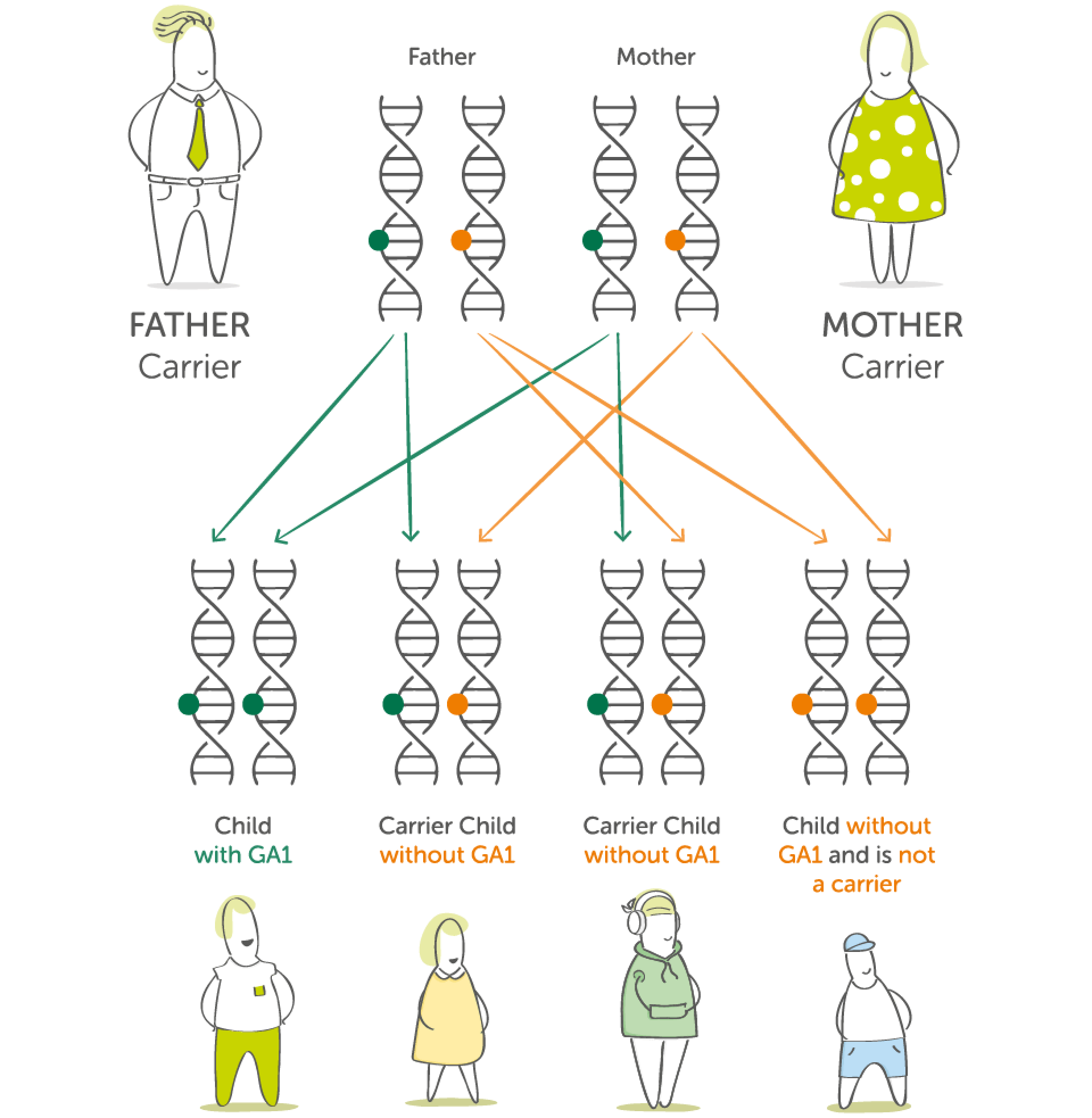
GA1 is an inherited genetic condition
It’s nobody’s fault and there is nothing you could have done to prevent it.
As a parent of a child with GA1, you have one GA1 gene and one unaffected gene.
This is known as being a carrier.
For a child to inherit GA1, it requires both parents to be carriers of the GA1 gene.
Your child has inherited 2 GA1 genes, one from the father and one from the mother and so therefore has GA1.
There are a small number of people who are carriers of the GA1 gene
People who are carriers for GA1 do not have GA1 themselves and in fact do not normally know they are carriers. The GA1 gene does not cause a problem to them.
When 2 people who are carriers for GA1 gene conceive a child, there is a 1 in 4 chance of that child having GA1.
The science bit... Protein explained
Why do we need protein?
Protein is one of the nutrients needed by the body.
It helps to build, repair and maintain body cells and tissues, like your skin, muscles, organs, blood and even bones.
Protein is made up of different building blocks called amino acids.
When it is eaten it is broken down into these amino acids so they can be absorbed into the blood stream and travel to where they are needed.
The conversion of protein into amino acids
Enzymes are special proteins which are like chemical scissors needed for the breakdown of protein into amino acids. There are 20 amino acids (building blocks) that make up protein.
Protein
Enzymes
Amino acids (Building Blocks)
Lysine and tryptophan are 2 of these amino acids and are used by the body to make new chemicals.
It is lysine and tryptophan that a person with GA1 cannot process correctly.
Why can someone with GA1 not process lysine and tryptophan correctly?
A person without GA1
Lysine and Tryptophan
Enzymes
Glutaric Acid
GCDH Enzyme
Energy + growth + repair
In a person without GA1 some of the lysine and tryptophan is broken down further to make glutaric acid and other chemicals.
Normally the liver produces an enzyme called glutaryl-CoA dehydrogenase (GCDH) which is used to convert glutaric acid to energy, which is used for growth and repair.
A person with GA1
Lysine and Tryptophan
Enzymes
Glutaric Acid
Faulty/No GCDH Enzyme
Buildup of glutaric acid and other harmful chemicals
In GA1 the conversion of glutaric acid into energy does not happen as it should. GCDH enzyme is either not made by the liver or it does not work properly.
This causes glutaric acid and other harmful chemicals to buildup.
Management of GA1…
- A protein restricted diet
- Protein substitute
- Medications – such as carnitine
- An Emergency Regimen during illness
Diet Management
A typical diet has too much protein for a person with GA1.
In GA1, it is important that enough protein is given for growth and development, but not too much as harmful chemicals will be made.
Therefore they must follow a protein restricted diet.
The diet will typically be made up as follows:
- Half - foods very low in protein
The remaining:
- Third - dairy based protein (i.e. yoghurt, cheese and milk)
- Third - cereal based protein (i.e. cereals and rice)
- Third - plant based protein (i.e. peas, sweetcorn and potatoes)
Measured amounts of protein
Your dietitian will advise you how much protein your child will tolerate.
This will depend on the severity of the condition.
These foods need to be measured and taken everyday.
They will mainly come from dairy, cereal and plant based foods.
Your dietitian will teach you how to measure protein.
They will provide you with a list of foods suitable for your child.
Low protein foods
Most fruit and vegetables such as, peppers, grapes, carrots and tomatoes can be eaten freely.
These foods should make up the majority of your child’s diet.
They provide an important source of energy and variety in the diet.
Your dietitian will provide you with a list of foods suitable for your child.
What is a protein substitute?
Why does a person with GA1 need to take a protein substitute?
Due to the protein restricted diet, some individuals may be unable to get all the nutrients they need by food alone. This is why a protein substitute* is essential.
A protein substitute is a specially made supplement. It is lysine free and has low levels of tryptophan, but it contains all the other amino acids in protein that your child needs to grow and develop.
Most protein substitutes also contain vitamins, minerals and other important nutrients to ensure your child is getting what they need.
The protein substitute helps control the buildup of toxic chemicals and protect the brain.
It is an extremely important part of the diet for a person with GA1.
It must be taken regularly and evenly spread over the day.
The protein substitute needs to be taken for the first 6 years of life and possibly for longer.
Your metabolic team metabolic team will discuss this with you in more detail.
* Protein substitutes designed for the dietary management of GA1 are Foods for Special Medical Purposes which must be used under medical supervision.
There are different protein substitutes which are designed to fit easily into everyday life and offer choice so that you find the right product to suit your child.
Your dietitian will advise you on which protein substitute is best for your child at each stage of their development.
The amount required will be calculated specifically for your child’s needs.
Always ensure you have a good supply of your protein substitute and medicines and that they are in date.
Management during illness
Emergency Regimen (ER)
As with all infants and children, illness will occur from time to time.
However, those with GA1 will need to start a special feed called the emergency regimen (ER) as soon as illness starts. DO NOT DELAY.
The ER is made up of a glucose polymer and a protein substitute.
Your child’s metabolic team will provide an emergency regimen specific for your child and will teach you in advance about what to do in times of illness.
This is an extremely important aspect of dietary management.
When your child gets ill, contact your child’s metabolic team immediately and keep in regular contact with them.
If symptoms continue and/or you are worried, go to the hospital immediately.
An ER can help minimise the impact of illness on your child.
Any common childhood illness or infection can cause glutaric acid levels to rise - avoidance of this is essential.
If left untreated, it can become life threatening.
The ER supplies energy and protein substitute to prevent a buildup of these harmful chemicals.
Always make sure you have your ER products and a written emergency plan - check that the products are in date.
It is important that your child continues to take their protein substitute during illness. Speak to your dietitian for advice.
During illness – start the ER promptly – do not delay
- Stop all protein in food and drink temporarily.
- Always complete the full amount of the emergency feed.
- Continue on medication as directed by your doctor.
- Maintaining your infant’s fluid intake during illness is important and extra fluid may be necessary.
- Keep in regular contact with your metabolic team.
How will I feed my newborn?
Infants: breastfeeding
Your infant will be given a lysine free, low tryptophan formula alongside the breastfeeds.
You will be advised by the dietitian on how much formula and breast milk to give.
Keeping a record of your infant’s intake may be useful.
Breastfeeding offers many benefits for infant and mother; it is recommended you discuss this with your healthcare professional.
Infants: bottle feeding
Your infant will be given a lysine free, low tryptophan formula in addition to a measured amount of the standard infant formula.
You will be advised by the dietitian on how much of each of the formulas to give.
Keeping a record of your infant’s intake may be useful.
Introducing complementary feeding and the second stage protein substitute to your infant
When to start introducing complementary feeding
Complementary feeding is often referred to as weaning. It is the process of gradually introducing solid foods into your infant’s diet. Your dietitian will advise you when to start solid foods, but it will occur around the same time as infants without GA1.
First foods introduced will initially be low protein foods.
This will help your infant to develop a healthy eating pattern while eating a variety of foods.
Your infant needs to continue to take their lysine free/low tryptophan formula and breast milk/ standard infant formula as advised by their dietitian.
This is also around the time that a second stage protein substitute may be introduced, your dietitian will advise you about this.
7 to 12 months
Once your infant is accepting low protein foods, some foods containing measured amounts of protein are introduced.
Over time, your child will get more of their protein from food (e.g. cereal) and replace the protein they were getting from breast milk or standard infant formula.
Your child will also be encouraged to move to more textured food and finger foods to encourage self-feeding.
Your infant will also begin to drink from a beaker.
Your dietitian will provide more detail about introducing complementary feeding and introducing the second stage protein substitute. Your dietitian will continue to advise you on your lysine free, low tryptophan formula / protein substitute intake.
Monitoring
You and your child will need to attend your specialist metabolic centre to meet with the metabolic team for ongoing monitoring and check-ups.
At your child’s monitoring visits, the team will spend time with you to ensure your child’s condition is being well managed and tailored to best suit the needs of your child and family.
To do this they look at many different factors such as:
- Your child’s overall health, growth and well-being.
- Blood tests - blood results give a good indication on how well your child is doing.
- Your child’s nutritional intake - it is helpful to bring diet diaries to your clinic visits.
Your dietitian and doctor will discuss any changes that may be needed to your child’s diet or medication.
It is very important to attend these monitoring visits. They will also give you opportunities to discuss concerns or questions you might have.
As your child grows up
Children / Teenagers / Adults
Following the prescribed diet, medication and acting quickly at times of illness ensures the best chance of a healthy life.
GA1 should not restrict your child or your family from fun activities, for example going on holiday and eating out.
Your child is most vulnerable in the first 6 years of life however your metabolic team may suggest your child continues the restricted protein diet, protein substitute and medication after the age of 6.
This will be discussed with you in greater detail.
Download to share offline
You can download and print an illustrated version of this page as a PDF which you can share with friends and family.
Browse other topics
Discover more from the comidamed world:



