An introduction to Phenylketonuria (PKU)
This easy to understand page will guide you through the early stages of a diagnosis to growing up.
This is an introduction to Phenylketonuria (PKU), following the diagnosis of your child with this condition.
Consult your metabolic team for diagnosis and treatment for PKU.
This page is not designed to replace any advice given by the metabolic team at the hospital.
If you are unclear about anything written here, please ask your dietitian for further information.
What is PKU?
Phenylketonuria or PKU for short (sounds like feen-il-ke-ton-u-re-ah)
- Children with PKU cannot use a part of protein called Phenylalanine (Phe).
- If left untreated, Phe builds up in the body and causes brain damage.
- This will be avoided by following a special diet.
- With proper management, people with PKU have every chance of attending university, building a successful career and enjoying a happy family life as everyone else.
Finding PKU early by screening, special dietary management and careful monitoring means that a child is able to reach their full potential.
Diagnosis of PKU
This blood test is carried out by a healthcare professional after birth. Once diagnosed a child will be referred to a specialist metabolic centre to ensure they receive the care they need.
Why does my child have PKU?
PKU is an inherited condition
It’s nobody’s fault and there is nothing you could have done to prevent it.
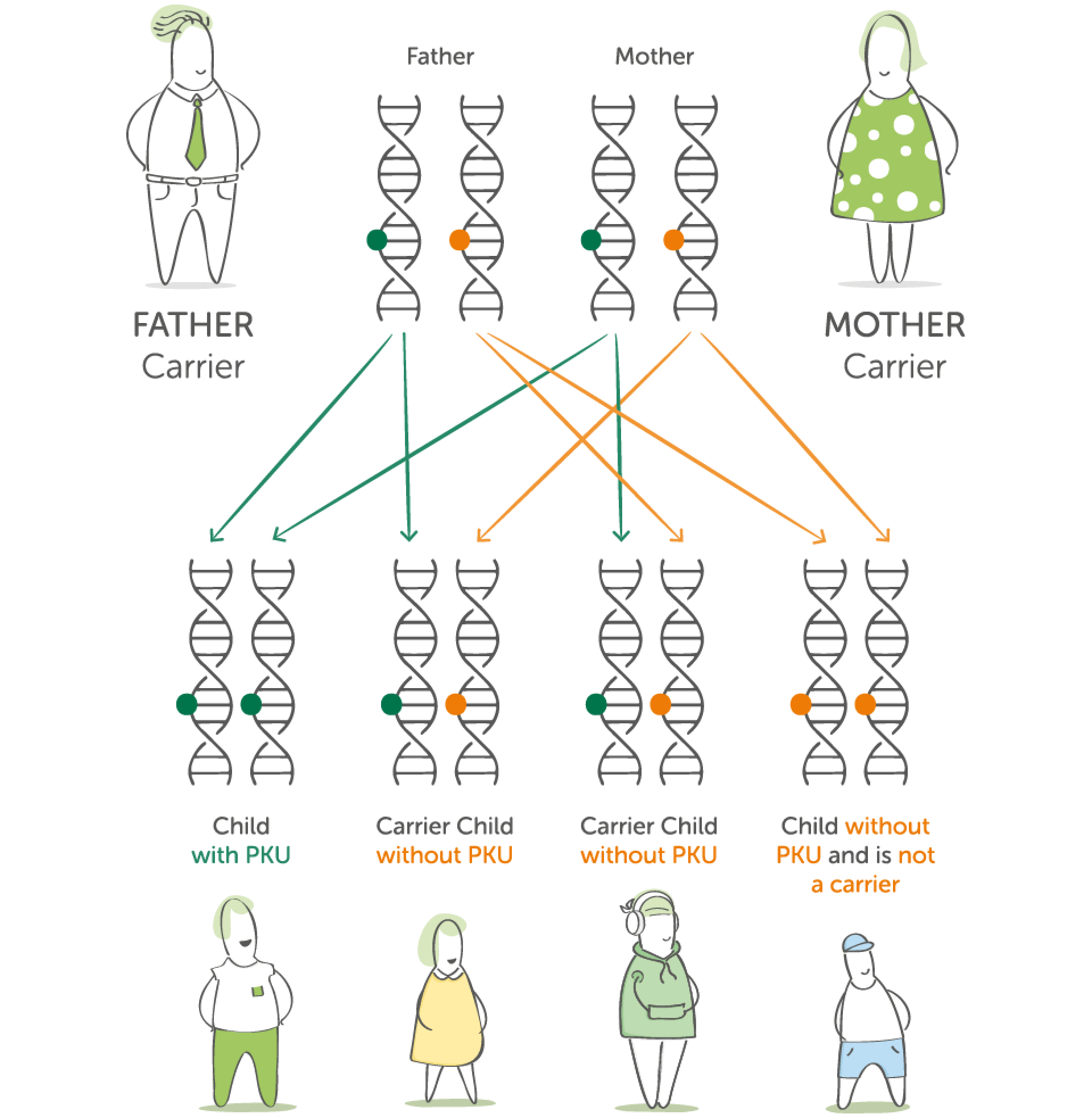
As a parent of a child with PKU, you have one PKU gene and one normal one. This is known as being a carrier.
Your child has inherited 2 PKU genes, one from the mother and one from the father.
Around 1 in 50 people are carriers of the PKU gene
People who are carriers for PKU do not have PKU themselves and the faulty gene does not cause a problem to them.
When 2 people who are carriers of the PKU gene conceive a child there is a 1 in 4 chance of that child having PKU.
The science bit... Protein explained
Why do we need protein?
Protein is a nutrient needed by the body.
It helps to build, repair and maintain body cells and tissues, like your skin, muscles, organs, blood and even bones.
When protein is eaten, it is broken down in the body (during digestion) into smaller pieces (like building blocks).
These smaller pieces are called amino acids.
Protein is made up of many building blocks called amino acids
There are 20 amino acids (building blocks) that make up protein.
Some of these are ESSENTIAL and cannot be made in the body - so they must come from the food we eat.
Phenylalanine (Phe) is one of these essential amino acids.
It is this particular amino acid that a person with PKU cannot process correctly.
What normally happens
The conversion of protein into amino acids:
Protein
Enzymes
Amino acids (Building Blocks)
Enzymes are like chemical scissors needed for the breakdown of protein into amino acids.
The body uses these amino acids for growing, building up muscle and helping the body stay healthy.
Why can someone with PKU not process Phe correctly?
A person without PKU
Phenylalanine (Phe) is converted into another amino acid called Tyrosine (Tyr).
Phenylananine (Phe)
Enzyme
Tyrosine (Tyr) is made
Normally, the liver produces an enzyme called Phenylalanine Hydroxylase. This enzyme breaks down Phenylalanine (Phe) to another chemical called Tyrosine (Tyr).
Tyrosine is important for many functions in the body.
A person with PKU
The conversion of Phenylalanine (Phe) into Tyrosine (Tyr) does not happen as it should.
Phenylalanine (Phe)
Faulty/No Enzyme
Little/No Tyrosine (Tyr) is made. This means there is a build up of Phe
In PKU, the enzyme phenylalanine hydroxylase is not made by the liver or the enzyme does not work properly. This means that Phe is not converted to the amino acid Tyrosine and builds up in the blood. This is the reason a special diet low in protein / Phe needs to be followed.
Low levels of Tyrosine also cause problems. Extra Tyrosine is therefore needed in the diet.
Management of PKU... the diet explained
A Regular Diet
A regular diet has too much protein / Phe for a person with PKU.
Therefore they must follow a special diet.
Management of PKU is by following a low protein / Phe diet
- Phenylalanine (Phe) is found in all protein containing foods, e.g. meat, fish, eggs, cheese, quorn, nuts, soya, pulses and in foods such as bread, biscuits and chocolate.
- In order to manage PKU, all protein foods must be restricted - and a low protein / Phe diet must be followed.
- All amino acids have a role or function in the body. Phe helps us with our growth, development and tissue repair.
- It is important that someone with PKU gets some Phe, but not so much that it becomes harmful.
Traffic Light System
The low protein / Phe diet a person with PKU must follow is best described by using the traffic light system:
Red: Stop!
- Too high in protein / Phe
- Do not eat these foods.
Amber: Go Cautiously!
- Contains some protein/Phe
- These foods can be eaten in measured amounts (exchanges).
Green: Go!
- Very low in / free from protein / Phe
- These foods can be eaten freely.
Red: Stop!
Do not eat the following foods:
- Meat
- Fish
- Cheese
- Tofu
- Nuts
- Pasta
- Bread
They are all rich in protein and therefore high in Phe so they are not allowed.
Amber: Go Cautiously!
Foods like potatoes, peas, cereal and rice can be eaten in measured amounts known as exchanges.
Other foods like these contain small amounts of protein. These foods can be eaten in measured amounts. The measure is called an exchange.
These foods are spread out between the day’s meals to provide small amounts of essential Phe. The quantities allowed will vary from person to person and from time to time in the same person.
Green: Go!
Foods such as peppers, grapes, lettuce, carrots, pears, sugar and oil can be eaten freely.
There are also special manufactured foods which are low protein:
- bread
- flour
- milk alternative
- chocolate flavoured bars
- pasta
- cereal
These foods are either naturally low in protein or have been specially made to be low in protein and so are “free from exchanges” or do not have to be measured*.
* please note certain specially manufactured low protein foods will need to be counted as part of phenylalanine exchanges. Please check with your dietitian.
What is a protein substitute?
Why does a person with PKU need to take a protein substitute?
- Due to restrictive nature of the diet, individuals are unable to get all the nutrients required by food alone. This is why a protein substitute** is essential.
- A protein substitute is a specially made medical supplement, which can come in various formats like a drink, a gel or tablets.
- A protein substitute contains NO Phe... But it contains all of the other amino acids in protein that your child needs.
- Most protein substitutes also contain vitamins, minerals and other important nutrients to ensure your child is getting what they need.
The protein substitute is a very important part of the diet for a person with PKU and it must be taken regularly and evenly spread over the day. This helps to keep the Phe levels steady through the day.
Your dietitian will discuss protein substitutes with you in more detail.
** Protein substitutes designed for the dietary management of PKU are Foods for Special Medical Purposes which must be used under medical supervision.
Protein Substitutes
Many protein substitutes are designed to fit into everyday life.
Your dietitian will advise you on which protein substitute is best for your child at each stage of their development.
How will I feed my newborn?
Infants: breastfeeding
Step 1
Once your child is diagnosed, you will be seen by a dietitian. Your infant will be given a Phe-free formula until the levels of Phe fall back to normal levels (usually within a few days).
Step 2
Once the levels of Phe are under control, a small amount of Phe-free formula is given before a breastfeed to restrict the amount of breast milk taken by the infant. Breast milk provides limited but essential Phe for normal growth.
Breastfeeding offers many benefits for infant and mother, it is recommended you discuss this with your healthcare professional.
Infants: non-breastfeeding (Bottle feeding)
Step 1
Once your child is diagnosed, you will be seen by a dietitian. Your infant will be given a Phe-free formula until the levels of Phe fall back to normal levels (usually within a few days).
Step 2
Once the levels of Phe are under control a small restricted amount of standard infant formula will be given along with the Phe-free formula to provide the limited Phe essential for normal growth.
Weaning
When to start weaning***
Your dietitian will advise you when to start solid foods, but it will be at the same time as infants without PKU.
These will initially be Phe free foods or foods that have a very low protein / Phe content.
This will help your child to develop a healthy eating pattern while eating a variety of fresh foods.
This is also the time that a second stage protein substitute may be introduced. Your dietitian will advise you about this.
*** Weaning may occur a little earlier than 6 months, depending on your infant but it should never be started before 17 weeks.
7 to 12 months
Your child will then be encouraged to move to more textured food and finger foods. Over time, they will get more of their Phe exchanges from food (e.g. potato or permitted cereal).
Less exchanges will come from breast milk or formula milk.
Phe free foods should still be included in the diet as well.
Your dietitian will continue to advise you on your phe free formula/protein substitute intake.
Monitoring
Your child will have regular blood tests and monitoring to make sure their Phe levels are under control. This is very important to ensure that they do not have too little or too much Phe in their diet.
Your dietitian will contact you once the results are processed and discuss any changes that may be needed to your child’s diet.
As your child grows up
Children / Teenagers / Adults
Your child will continue to follow a low protein / Phe diet as they grow up into adulthood.
You, your child and dietitian will help choose the protein substitute that best suits them and their lifestyle.
Download to share offline
A family friendly version of this information is available as a colourful PDF, which you can download and print.
Browse other topics
Discover more from the comidamed world:



